Conditions & Treatment Options
Substance use and mental health (dual diagnosis)

In this section we have information on how certain substances affect the body along with diagnosis concerns and the recovery process. A list of recommended resources is also available.
for Consumers
02. To assist discussion about treatment, discharge planning and post discharge support across mental health and AOD, look at Consumers Can Ask
03. There are a number of peer support groups available including those run by SHARC, SMART Recovery, AA, and NA.
04. Talk to your local GP, or your local community health AOD service.
for Carers
02. Family Drug Help (SHARC) provides practical help, information and support to families and friends. Their helpline is 1300 660 068
03. SHARC also offer the InFocus Education Program: A community-based psychoeducational program for families and friends affected by someone’s AOD use.
04. The National Carer Gateway outlines respite and financial options, carer support including practical resources, and life stories.
Dual issue?
Dual diagnosis is when a person experiences mental health issues and also uses alcohol and/or other drugs. Dual diagnosis is very common.
When we talk about substances we mean both legal and illegal substances that affect the mind, i.e. alcohol, tobacco, cannabis, amphetamines, and so on.
People have used substances for thousands of years, and substance use in one form or another remains very much part of most cultures.
People use substances for many reasons. Most people use substances to enjoy the experience and feel good. Unfortunately, using substances can also cause problems, or unwanted experiences or effects.
It is estimated that anywhere between 40 – 80% of consumers/service users who experience mental illness also have issues with substance use and vice versa. At most treatment services, dual diagnosis is the rule rather than the exception.
Remember that your mental health and substance use can impact on each other, so it can often be helpful to seek assistance for both challenges at the same time.
It can be very stressful when a loved one is experiencing difficulties with their mental health and substance use. Often, the people closest to them, such as family, friends or carers, can find it difficult to know how to help and how to access services for both their loved on and themselves.
Many services offer assistance to a person’s family to help them understand what is going on, what sort of treatments are being provided and how they can best provide support and assistance. Have a look at our carer resources at the top of this page to get you started.
Substance use and mental health (dual diagnosis)
Frequently asked questions (FAQs)
What is dual diagnosis?
What are the patterns of use?
- Experimental use is defined as trying a substance for the first time, and is usually infrequent. Experimental use can still be unsafe. For example, there is a risk of overdose, particularly when your body is not used to the substance. Experimental use can also lead to more frequent use, needing more and more of the substance to get an effect, and dependence.
- Recreational use is defined as regular use in particular settings. For example, drinking alcohol when out with friends.
- Bingeing is defined as heavy use of a substance within a short space of time. Bingeing is associated with specific risks including accidental overdose (especially when other substances are combined).
- Dependence usually occurs when a person is using a substance regularly and in high amounts. A person who is dependent can tolerate much higher doses of the substance, tends to experience withdrawal symptoms when they are not using the substance, and spend a lot of time, energy, and money, getting and using the substance.
Is it common to experience dual diagnosis?
Services funded through the Department of Health are mandated to work with consumers with a dual diagnosis.
How does dual diagnosis affect you?
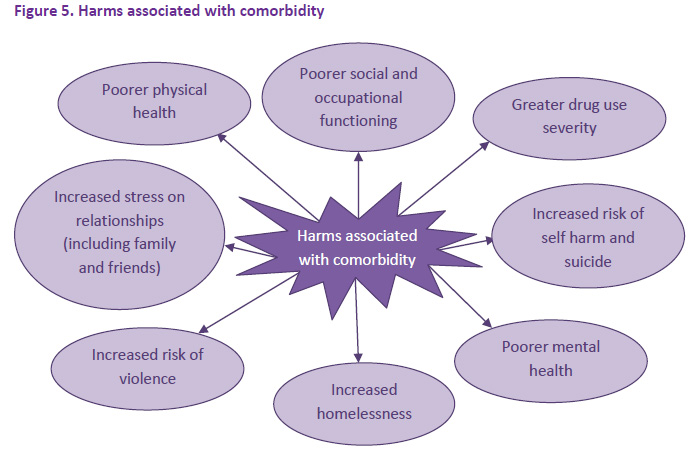
There are a number of harms linked to dual diagnosis. Some of these are depicted below. NDARC Comorbidity Guidelines (click for larger view)
However, it’s also known that earlier and appropriate treatment results in:
- Lower rates of relapse, hospitalisations and use of emergency services
- Increased adherence to treatment
- Decreased rate of offending and reduced likelihood of incarceration
- Reduction in positive symptoms (delusions/hallucinations/thought disorder)
- Reduced risk of suicide and early mortality
- Increased stability in areas such as housing, employment, and personal relationships
- Increased quality of life and personal wellbeing
- Better overall functioning and engagement with family, friends and community
How should dual diagnosis be treated?
In Victoria, all AOD and Mental Health Services (Clinical services and Mental Health Community Support Services (MHCSS)) are encouraged to provide integrated treatment.
People experience Dual Diagnosis in different ways, and many people will respond to different treatment options. It is important to persevere and find the treatment that works the best for you. It’s also a good idea to check that your services are all talking to one another.
Where do I get help for dual diagnosis?
Where and how you participate in this treatment depends on many different factors, including what makes you more comfortable and what you feel works.
Both Mental Health Services and Alcohol and Other Drugs Services are funded to treat Dual Diagnosis as their core business. Speak with your case manager or counsellor about what types of assistance they can provide you with, or where to find other forms of support.
What is the recovery process for dual diagnosis?
Building a rewarding and meaningful life without substances can take time time, support, education, courage and the learning of new skills. While families and clinicians can help in the recovery process by providing support and hope, recovery is the person’s own choice.
What are the family and carers issues?
Many services offer assistance to a person’s family to help them understand what is going on, what sort of treatments are being provided and how they can best provide support and assistance. Have a look at our carer resources at the top of this page to get you started.
Resources
Types of substances
| Type | How they affect your body |
|---|---|
| Depressants | Slow down messages from the brain, for example:
|
| Stimulants | Speed up messages from the brain, for example:
|
| Hallucinogens | Change the way messages are interpreted by the brain, for example:
|
Some substances can have mixed effects. The effects that you experience can be affected by many factors including how much you take, your body size, level of fitness, and how you take it.
Using more than one substance at any time can alter the effects and can dramatically increase the risks.
To find more about specific drugs and their effects, visit the Australian Drug Foundation for more information.
Recommended resources
Directline: 24hr confidential alcohol and other drug (AOD) counselling and referral in Victoria for consumers, carers and workers. 1800 888 236
Alcohol and other Drugs (AOD) Pathways is a Victorian based state-wide service that aims to support individuals and their significant others to navigate and access local AOD treatment services. 1800 319 619
Dual diagnosis residential rehabilitation beds are now available in Victoria. Further information is available in this information sheet.
* Sources: Ref: SUMITT DDx leaflet | Ref: Lincoln Dual Diagnosis Manual, 2007. | Ref: NDARC Comorbidity Guidelines
With special thanks to
Many people have contributed to the development of this project through research, focus groups, advice, information and ideas. We would like to acknowledge and thank all who have contributed and supported us in our endeavor. They are:
Chris Hynan, Dr Kah-Seong Loke, Merissa van Setten, Adrian Fitt, Ange Wallace, Kevan Myers, Lynne Ruggiero, Sarah Officer and Simon Kroes
Newsletters
Stay in the loop with our monthly newsletters!
If you are having thoughts of suicide, or severe self-harm please follow your crisis plan. If you do not have a crisis plan please call your treating clinician, therapist, general practitioner, one of the numbers listed below or go to the Emergency Department of the nearest hospital. In a life-threatening emergency ring 000.
Phone numbers and other supports that can be contacted in a crisis:
Life Line: 13 11 14 | www.lifeline.org.au
Sane Helpline: 1800 187 263 | www.sane.org




 The 2014 Act came into effect in July 2014. It introduced new principles to support people experiencing mental illness to make and participate in treatment decision (shared decision making) and to have their views and preferences considered and respected.
The 2014 Act came into effect in July 2014. It introduced new principles to support people experiencing mental illness to make and participate in treatment decision (shared decision making) and to have their views and preferences considered and respected.