Conditions & Treatment Options
Schizophrenia

In this section we explore how diagnosis is made and how antipsychotic medications work. Electroconvulsive therapy is also explained and other methods of managing schizophrenia.
What is schizophrenia?
A psychotic disorder involves a disconnection from reality. Psychosis is a group of related symptoms that seriously affect how you think, feel, and behave.
Schizophrenia is a mental disorder characterised by disruption in thoughts, emotions, behaviour, reality testing, and cognitive functioning causing significant distress to the person or decline in the capacity to function.
Helplines
01. Beyond Blue Helpline: 1300 224 636
02. SANE Helpline: 1800 18 SANE | 1800 18 7263
04. MensLine Australia Helpline: 1300 789 978
05. Headspace Helpline: 1800 650 890
06. Healthdirect Australia Helpline: 1800 022 222
Taking action for change. You can come up with an individual treatment and support plan with the help of your GP and specialist mental health professionals, such as psychiatrists or mental health caseworkers. Involving your family as well can be helpful. You can use the National Health Services Directory to find a health professional near you.
Schizophrenia
Frequently asked questions (FAQs)
What’s schizophrenia and how does it present?
The disruption in thoughts can present through speech as muddled thinking, the mind going blank, or mixing unrelated topics in a way that is difficult to follow. In extreme cases, thoughts can be completely illogical and incomprehensible. Sometimes a person with schizophrenia can have inappropriate emotional reactions to situations, like being completely indifferent and untouched by different events or may have inappropriate reaction like smiling and being happy when told sad news, and vice versa.
In terms of the behaviour, this can be a disorganised behaviour or bizarre, like being mute, posturing, repeating actions and phrases of others automatically, etc.
Impaired reality testing can manifest with delusions (inappropriately fixed beliefs held despite evidence to the contrary) or hallucinations (a perception without a real stimulus). An example of a delusion would be paranoid delusions of people being after the person without a real reason behind this. Delusions can be in many themes, including guilt, grandiosity, poverty, etc. Hallucinations can be in any of the five senses (visual, auditory, olfactory, gustatory and tactile (taste, smell and touch). Hallucinations and delusions are usually referred to as the positive symptoms of schizophrenia. On the other hand, the deficit-like presentation is usually referred to as the negative symptoms and usually presents with slowed thought process, slowed movement, lacking initiative and lacking interest in participating in any activities (without being depressed).
How is the diagnosis made?
A Two or more of the following lasting for a month:
- Delusions
- Hallucinations
- Disorganised speech
- Disorganised behaviour
- Negative symptoms
B Significant impairment in functioning
C Six months duration of disturbance to include one month of symptoms from group A and any disturbance from usual self for the remaining of the six months which can include mild form of the symptoms of schizophrenia1.
What causes schizophrenia?
Are there antipsychotic medications available for schizophrenia?
Medications:
Antipsychotic medications are usually recommended as part of the treatment of psychosis to assist in recovery and prevent further relapse. There are a number of antipsychotic medications available and choice needs to be personalized to ensure the best tolerability and efficacy. Where possible, the strategy should be to start the antipsychotic at a low dose and gradually in-crease to minimize any side effects.
Benzodiazepines are often useful as short-term addition to the antipsychotic medication during an acute episode since they reduce agitation, tension and anxiety and help with sleep. However, care should be taken to avoid using them for more than 4 weeks due it their addictive nature.
Antipsychotic medications can be taken orally or given as a depot (long-acting injection).
There are two groups of antipsychotic medications:
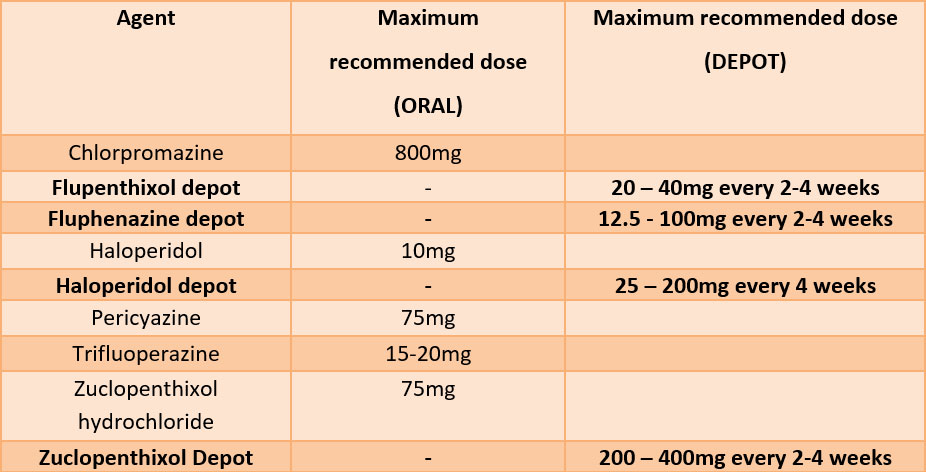
1. Typical or First Generation Antipsychotics (Australia):
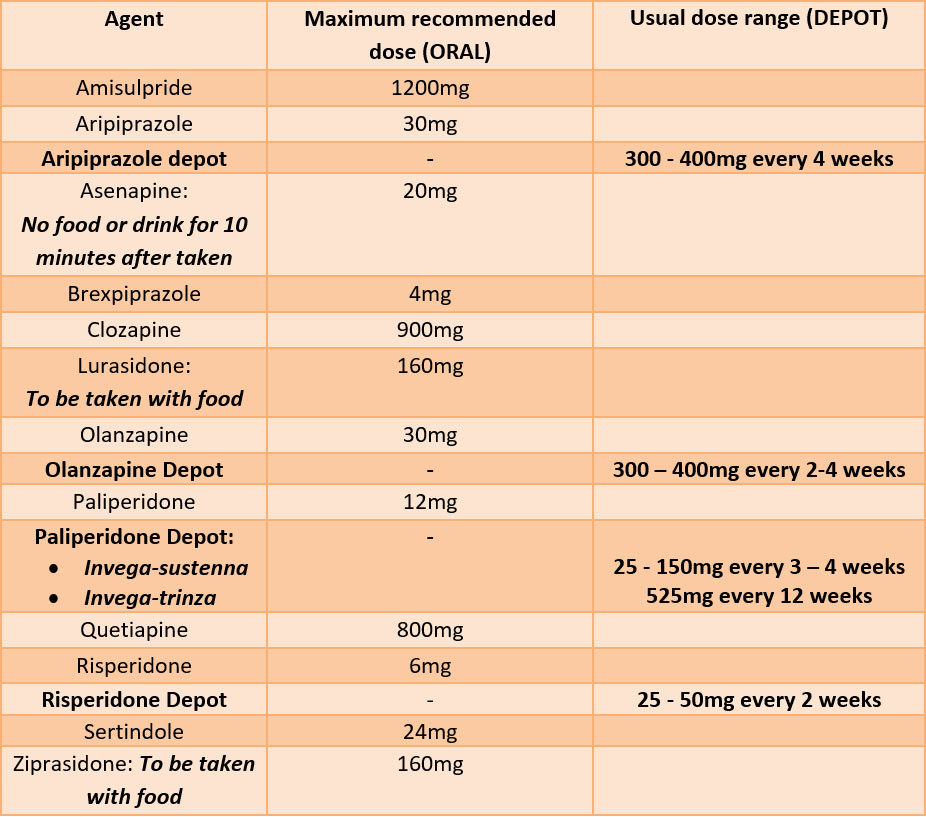
2. Atypical or Second Generation Antipsychotics (Australia)
All antipsychotics are effective in reducing or eliminating positive symptoms of psychotic disorders; however, the atypical or second generation antipsychotics generally have less tendency to cause movement disorder side effects (“extrapyramidal side effects = EPSE) such as rigidity, persistent muscle spasm, tremors and restlessness. Furthermore, they may be effective in improving mood, thinking and motivation.
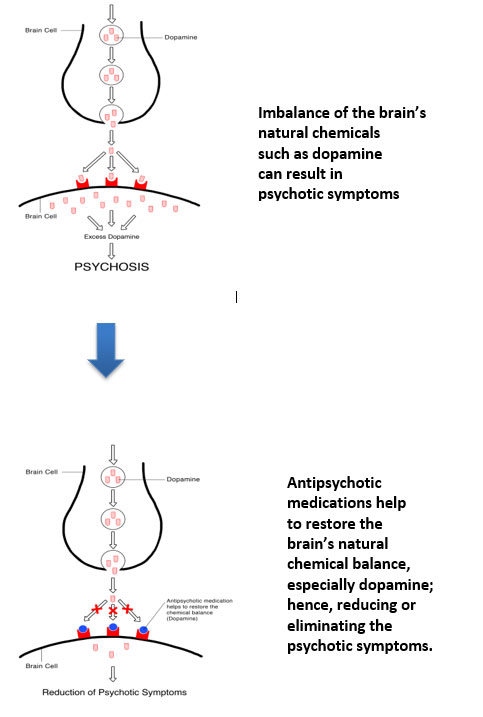
How do antipsychotic medications work?
How do you manage antipsychotic medications?
Antipsychotic medications begin to relieve agitation and sleep disturbances in about one week. Many people see substantial improvement by the fourth to sixth week of treatment. Do not decrease or increase the dose or stop the antipsychotic medication without discussing with your doctor first.
Why it is so important to keep taking them?
Antipsychotic medications reduce the risk of future psychotic episodes in people who have recovered from an acute psychotic episode. Even with continued drug treatment, some people who have recovered will suffer relapses. Because relapse of schizophrenia is more likely when antipsychotic medications are discontinued or taken irregularly, it is very important that people with schizophrenia work with their doctors and family members to adhere to their treatment plan.
Good adherence involves taking prescribed antipsychotic medication at the correct dose and proper times each day, attending clinic appointments, and/or carefully following other treatment procedures. Treatment adherence is often difficult for people with schizophrenia, but it can be made easier with the help of several strategies and can lead to improved quality of life.
How long should I take this medication?
Following a first episode of psychosis, it is recommended that antipsychotic medication can be continued for at least 1 -2 years; this decreases the chance of becoming ill again.
For individuals that have had a psychotic illness for several years or repeated psychotic episodes, antipsychotic medication should be continued indefinitely. This is similar to someone with diabetes requiring lifelong insulin.
What happens if a dose is missed?
Take the missed dose as soon as possible, as long as it is only a few hours after the usual time. Otherwise, wait until the next dose is due and take it as normal.
Do antipsychotic medications have any unpleasant side effects?
The long-term side-effects of antipsychotic medications such as tardive dyskinesia (a disorder characterised by involuntary movements most often affecting the mouth, lips, and tongue, and sometimes the trunk or other parts of the body such as arms and legs. It occurs in about 15 to 20 percent of individuals who have been receiving the older, “typical or first generation” antipsychotic medications for many years.
‘Atypical or second generation” antipsychotic medications all appear to have a much lower risk of producing tardive dyskinesia (TD) than the older, traditional antipsychotics. However, they can produce side-effects of their own such as weight gain, which may place individuals treated with antipsychotics at risk of metabolic side-effects (“metabolic syndromes”). It is recommended that metabolic monitoring should be carried out regularly to all individuals who are taking psychotropic medications.
Do antipsychotic medications interact with cigarette smoking?
Source: St Vincent’s Psychiatric medication information: A guide for patients & carers 4th Edition, 2017.
What is Electroconvulsive Therapy (ECT)?
– bipolar disorder
– schizophrenia
– catatonia
ECT is not typically recommended as the first option of treatment. It is prescribed when medications do not work, or when an individual cannot take medications due to the severity of side effects or another medical condition. It can be recommended when a person requires rapid treatment because they are at risk of suicide.
What psychological treatment:s are available?
Structured time limited psychotherapy involving the here and now focusing on strategies to cope with the chronic and treatment resistant delusions and hallucinations.
Family therapy:
Family intervention to help the family to understand more about the illness and how best to support the family member with schizophrenia without adding more stress on the family as a unit and the individual with schizophrenia.
Others:
cognitive remediation therapy, supportive therapy, etc.
Are there social interventions and other methods of managing schizophrenia?
– Social skills training
– Vocational training
– Social support
Managing schizophrenia usually involves a team of different disciplines (i.e., a multidisciplinary team) to provide a holistic approach to the care and support while ensuring community follow up and monitoring of mental state. At times, the illness can take a severe form with total loss of reality testing, self-harm, suicidal thoughts or even thoughts of harming others. In such cases, admissions can be necessary and in rare cases, electroconvulsive therapy may be considered.
What is the outlook?
Resources
Recommended resources
A national initiative operated by Healthdirect Australia, on behalf of the Australian Federal Government as part National E-Mental Health Strategy. You can access a range of mental health resources including online programs, fact sheets, audio and video, and online communities.
Beyond Blue www.beyondblue.org.au Helpline: 1300 224 636
Non-government organisation which provides extensive information about depression, anxiety and related mood disorders across various stages of life and areas of the community.
SANE www.sane.org.au Helpline: 1800 18 SANE | 1800 18 7263
SANE Australia was founded in 1986. It I a national charity helping all Australian affected mental illness lead a better life – though campaigning, education and research.
Black Dog Institute www.blackdoginstitute.org.au
The Black Dog Institute was launched in 2002. It offers specialist expertise in mood disorders (depression and bipolar disorder) and also acts as an umbrella organisation, supporting a range of programs that focus on mood disorders.
myDr myDr.com.au
myDr provides free comprehensive easy-to -understand Australian health and medicines information for consumers (CMI)
MensLine Australia www.mensline.org.au Helpline: 1300 789 978
MensLine Australia is a national support, information and referral services for men across Australia, specialising in family and relationship concerns.
ReachOut www.reachout.com www.reachout.com/schizophrenia
ReachOut.com is Australia’s leading online youth mental health service with a mobile-friendly site and forums which consumer can access help, information and support.
Headspace www.headspace.org.au Helpline: 1800 650 890 Headspace psychosis toolkit
Headspace established in 2006. It is the National Youth Mental Health Foundation, which provides mental health wellbeing support, information and services to young people ages 12 to 25 years and their families.
Healthdirect Australia www.healthdirect.gov.au Helpline: 1800 022 222
Healthdirect provides Australians with access to trusted health information. All information has been provided through partnerships with government agencies and other trusted sources.
This Way Up www.thiswayup.org.au
This Way Up provides research tested online treatment and prevention of depressive and anxiety disorders. It is a not-for-profit initiative of St Vincent’s Hospital, Sydney and the Faculty of Medicine at University of New South Wales.
1 APA. DSM-5 2013.
2 O’Donovan MC, Williams NM, Owen MJ. Recent advances in the genetics of schizophrenia. Hum Mol Genet. 2003(2):2.
3 Gregg L, Barrowclough C, Haddock G. Reasons for increased substance use in psychosis. Clin Psychol Rev. 2007;27(4):494-510.
4 Selten JP, Cantor-Graae E, Kahn RS. Migration and schizophrenia. Curr Opin Psychiatry. 2007;20(2):111-5
5 van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635-45.
6 Menezes NM, Arenovich T, Zipursky RB. A systematic review of longitudinal outcome studies of first-episode psychosis. Psychol Med. 2006;36(10):1349-62.
With special thanks to
Many people have contributed to the development of this project through research, focus groups, advice, information and ideas. We would like to acknowledge and thank all who have contributed and supported us in our endeavor. They are:
Newsletters
Stay in the loop with our monthly newsletters!
If you are having thoughts of suicide, or severe self-harm please follow your crisis plan. If you do not have a crisis plan please call your treating clinician, therapist, general practitioner, one of the numbers listed below or go to the Emergency Department of the nearest hospital. In a life-threatening emergency ring 000.
Phone numbers and other supports that can be contacted in a crisis:
Life Line: 13 11 14 | www.lifeline.org.au
Sane Helpline: 1800 187 263 | www.sane.org




 The 2014 Act came into effect in July 2014. It introduced new principles to support people experiencing mental illness to make and participate in treatment decision (shared decision making) and to have their views and preferences considered and respected.
The 2014 Act came into effect in July 2014. It introduced new principles to support people experiencing mental illness to make and participate in treatment decision (shared decision making) and to have their views and preferences considered and respected.